Men's Health: Early Prostate Cancer Detection Leads to Better Outcomes
Author
South Shore Health
November is Men's Health Awareness Month, a time to highlight health issues affecting men – including prostate cancer.
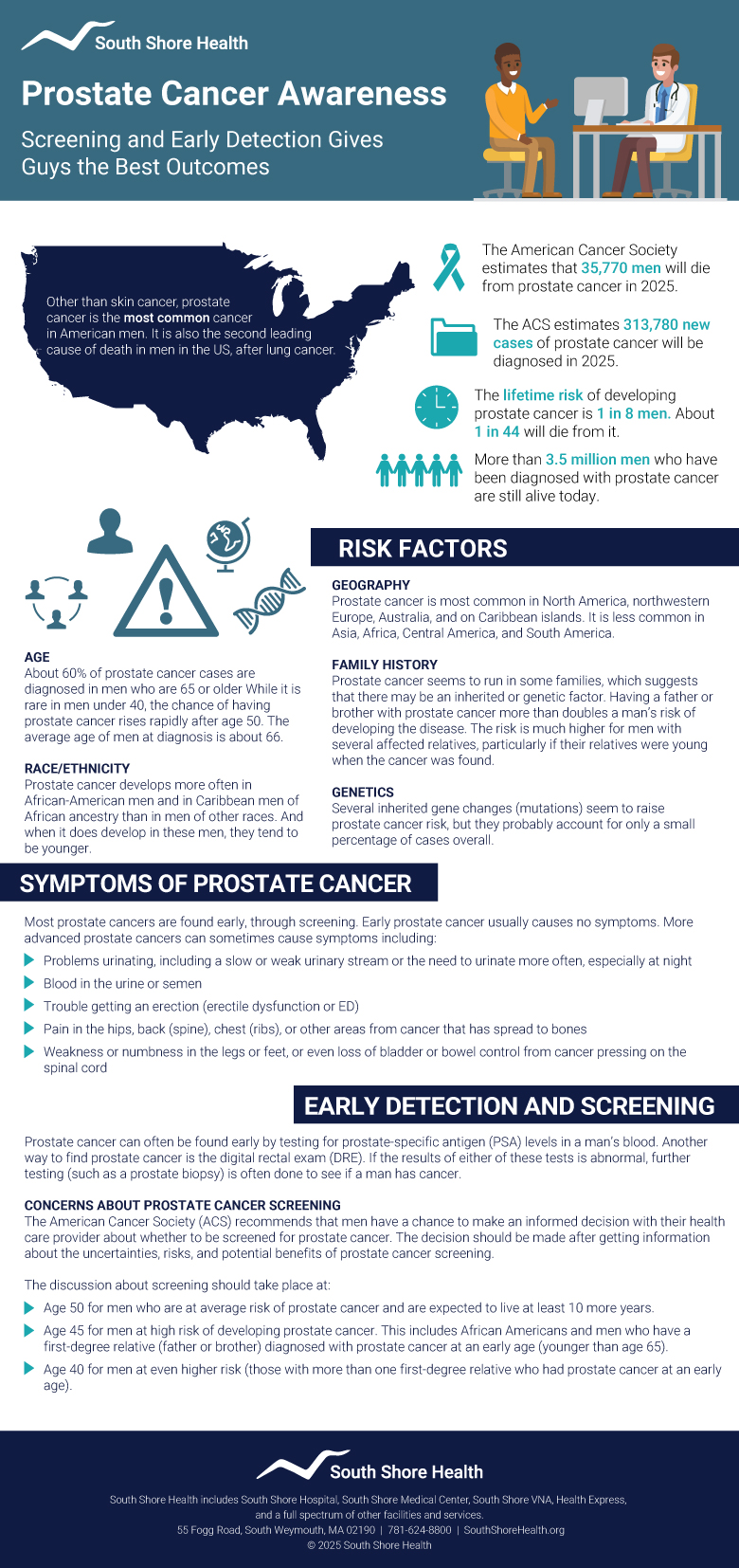
Prostate cancer is the second most common cancer affecting American men and the second most common cause of cancer death for men.
According to the American Cancer Society (ACS), about 313,780 new cases of prostate cancer will be diagnosed in 2025 and 35,770 men will die from the disease.
A disease generally affecting older men – 6 in 10 cases are diagnosed at 65 years or older – prostate cancer is rare in men under age 40. But incidence rates have been on the rise in the last decade, increasing by 3% annually.
Because there are often no symptoms associated with early-stage prostate cancer, screening is crucial for early detection, better treatment options and more favorable outcomes for men.
Radiation oncologist Peter F. Orio, III, DO and Chief of Urology Sergio D. Fefer, MD answer questions about risk factors, symptoms, treatment and the screening tests that help catch prostate cancer early when it’s easier to treat.
Why is routine screening for prostate cancer so important?
Orio: Many men with early-stage prostate cancer never experience symptoms and without screening, would never know that they have the disease. Because of this, screening protocols, typically with prostate-specific antigen (PSA), are critically important for early detection as they allow men to be diagnosed with prostate cancer many years before it becomes problematic.
Fefer: Prostate cancer is a very prevalent disease that is not preventable and due to its paucity of symptoms, has been usually diagnosed at an advanced stage. Since the introduction of PSA testing as part of the routine physical exam, there has been a shift to diagnose prostate cancer at an earlier stage, which translates into a better outcome through earlier interventions.
What kind of screening is available for prostate cancer and at what age should men start?
Orio: Periodic PSA-based testing and physical exams are the two most common prostate cancer screenings available for men today. In 2018 the U.S. Preventive Services Task Force suggested that screening begin for men aged 55 to 69 years, however the decision to undergo PSA-based screening for prostate cancer should be an individual one based on the risk of harboring malignancy an often starts at earlier ages.
Before deciding whether to be screened, men should have an opportunity to discuss the potential benefits and harms of screening with their clinician and to incorporate their values and preferences in the decision. In determining whether screening is appropriate in individual cases, patients and clinicians should consider the balance of benefits and harms on the basis of family history, race/ethnicity, comorbid medical conditions, patient values about the benefits and harms of screening and treatment-specific outcomes, and other health needs.
Fefer: I fully agree with Dr. Orio. After discussing the pros and cons of screening with my patients, I frequently recommend to start checking PSA and to do a prostate exam at age 50, for healthy individuals without a family history of prostate cancer. For men with a first-degree relative diagnosed with prostate cancer before age 60, I recommend to begin screening in the mid 40s. New data suggest that checking PSA level once on the mid 40s could be beneficial for patients without risk factors as well.
What are some of the risk factors for prostate cancer and are there lifestyle changes that can lower the risk?
Orio: Approximately one in eight men will be diagnosed with prostate cancer during his lifetime, and it accounts for nearly 10% of all newly diagnosed malignancies among men. Prostate cancer is rare in men younger than 40, but the chance of having prostate cancer rises drastically after age 50.
African American men and men with a family history of prostate cancer have an increased risk compared with other men. Having a father or brother with prostate cancer nearly doubles a man’s risk of developing this disease.
Fefer: Age, African American race, and first-degree relative with prostate cancer are known risk factors for prostate cancer. There is ongoing research about the influence of diet on the risk of getting prostate cancer but there are no conclusive results that can be applied at the present time.
What are some symptoms of prostate cancer that should be discussed with a health care provider?
Orio: In the early stages of prostate cancer most men do not have any symptoms associated with their malignancy, which is what makes screening protocols critical. However, in more advanced stages of prostate cancer men can experience difficulties urinating due to the prostate cancer obstructing the urethra, which is the tube that empties the bladder and goes directly through the prostate.
Although obstructive urinary symptoms can be the result of a benign enlargement of the prostate, symptoms such as a weak urinary stream, straining with urination and the need to urinate frequently and urgently should be discussed with a physician to make sure they are not associated with prostate cancer.
In the very late stages of untreated prostate cancer men can present with bone pain associated with the cancer traveling from the prostate and metastasizing to the bone.
Fefer: Prostate cancer tends to be a silent disease with barely any symptoms, but as the disease progresses some manifestations include worsening urinary symptoms, blood in the urine, and pelvic or bone pain.
What kind of treatment options are available for someone diagnosed with prostate cancer?
Orio: Several treatment options exist for prostate cancer, including surgery, external beam radiation therapy, brachytherapy and hormonal therapy. Choosing the right treatment option is highly individualized and can be confusing for men and physicians alike.
In choosing the treatment option that is right for them, men should seek medical advice from their urologist, as well as a radiation oncologist and medical oncologist to hear all of their options.
In health care, knowledge is power and a patient should always be provided both the power and knowledge to make informed decisions in the treatments they elect and receive.
Fefer: Prostate cancer is not a single disease but a spectrum that ranges from an indolent tumor with excellent prognosis that requires no other treatment than periodic surveillance, to an aggressive cancer that requires aggressive treatment either with surgery or with radiation.
In some cases, treatment includes both surgery and radiation and many times a hormonal treatment androgen deprivation – is added to enhance the response to treatment.
Due to the complexity of the disease and the different treatment modalities, men newly diagnosed with prostate cancer should be evaluated by a multidisciplinary approach including an urologist, medical oncologist, radiation oncologist, and geneticist.
Peter F Orio, III DO, MS, FABS, FASTRO is Chair of Dana Farber Radiation Oncology and sees patients at the Dana-Farber Brigham Cancer Center at South Shore Health. He is an Associate Professor of Radiation Oncology at Harvard Medical School. Learn more about prostate cancer care and radiation oncology at the Cancer Center.
Sergio D. Fefer, MD is Chief of Urology at South Shore Health and is in practice at South Shore Urology in Weymouth. Learn more about genitourinary care at South Shore Health.
Author
South Shore Health