It’s OK to be Over COVID – ‘We’re in a Better Place'
Author
South Shore Health
Four years ago this month our world shut down in response to the rapidly spreading COVID-19 virus.
Schools and businesses closed and millions of people stayed home, isolating themselves from others to avoid exposure to this new and potentially deadly, respiratory illness.
We’ve come a long way since those early, uncertain days of the pandemic.
So far in fact, that many people have only faint memories of the long periods of lockdown spent streaming “Tiger King,” piecing puzzles together and longing to eat out at a restaurant again.
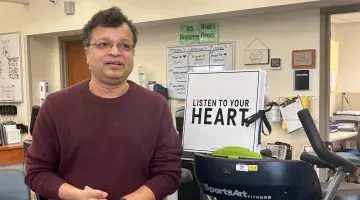
Most people have moved on from COVID-19 and that’s okay, even though COVID-19 isn’t over, said Todd Ellerin, MD, South Shore Health’s Director of Infectious Disease.
“We’re in a completely, 180-degree different place than we were four years ago,” said Ellerin, who weighed in on the updated COVID-19 guidance the Centers for Disease Control and Prevention (CDC) recently issued.
In the first changes to its COVID-19 isolation guidelines since 2021, the CDC announced March 1, it was shortening the time people should isolate following COVID-19 infection, matching it to other respiratory illnesses – including RSV or the flu. The revision recognizes the similarities of symptoms, means of spread and containment strategies for these respiratory viruses, according to the CDC.
The new guidance recommends that people who are sick with a respiratory virus stay home and away from others until their symptoms have improved overall and they have been fever-free without the use of fever-reducing medications for at least 24 hours.
After resuming normal activities, people are encouraged to take additional infection prevention steps including frequent handwashing, wearing a well-fitting mask for five days (down from 10 days), keeping a distance from others and/or getting tested for respiratory viruses.
Ellerin said the updated CDC recommendations make sense for where we are now with respiratory viruses.
“Four years ago we had hundreds of thousands of high-risk patients dying amid a once-in-a-century respiratory pandemic. Today, hospitalizations and deaths are way down."
The third leading cause of death in the U.S. (after cancer and heart disease) in 2021, COVID-19 dropped to tenth in 2023, and deaths due to the virus decreased 83% during that period, according to CDC data.
The updated guidance on isolation is indicative of the progress we’ve made in preventing, treating and living with COVID-19, Ellerin said. And the unification of these prevention strategies, should make the recommendations easier for people to follow and adopt.
“While the contagious period for COVID-19 hasn’t changed, the risks of keeping kids out of school and people out of work, outweigh the benefits of reduced spread of infection now that we have greater population immunity and access to effective antiviral medications for high risk individuals,” he said.
The CDC estimates that more than 98 percent of the U.S. population has some degree of protective immunity against COVID-19 from vaccination, prior infection, or both.
“Our immune system is really smart and is on our side in this.”
Still, Ellerin stressed the importance of keeping up with COVID-19 vaccines and testing for the virus if you’re high risk for serious illness, or plan to visit someone who is.
Both COVID-19 testing and vaccination numbers have declined sharply in the past year.
It’s estimated that less than 50% of people are still testing for COVID-19, and according to the CDC, only 22% of adults and 12% of children have received the latest COVID-19 vaccine released last September.
Along with its new guidelines for isolation, the CDC Advisory Committee on Immunization Practices (ACIP) has recommended adults 65 and older get an additional dose of the new COVID-19 vaccine this spring, as protection from shots received last fall may have waned.
“For higher risk groups it makes sense to get a second vaccine in the spring,” Ellerin said. “For most people, as with the flu vaccine, one shot per year in the fall is enough.”
“We’re in a better place now, but COVID-19 is still causing mortality,” he said, noting that roughly 100,000 people in the U.S are dying due to the virus each year.
And yet four years after the pandemic began, there’s reason for optimism for the future, and reflection on just how far we’ve come with COVID-19, Ellerin said.
“We know COVID continues to mutate and change and it’s not going to stop that,” Ellerin said. “But we’ve lived with it for four years and have developed anti-viral treatments that work irrespective of the virus strain. And we have effective vaccines that can lower the chance of infection and significantly prevent severe illness.”
When you consider how the world has worked together to take on COVID-19, it’s an amazing story of courage and resilience, he said.
Todd B. Ellerin, MD is Director of Infectious Disease at South Shore Health.
Author
South Shore Health