Palliative Care Team Supports Patients and Families Navigating Serious Illness
Author

Alyson Hawkins, PA-C
November is National Hospice and Palliative Care Month, a time to raise awareness about this specialized care and to recognize the dedicated caregivers and professionals committed to providing comfort and support to patients with serious, chronic and/or life-limiting illnesses.
Palliative care provider Alyson Hawkins, PA-C, explains more about palliative care and the important role South Shore Hospital’s Palliative Care Team plays in improving the lives of patients and families.
What is palliative care?
Palliative care is a medical specialty that provides symptom relief and support to patients with a serious, chronic or life-limiting illness. Palliative care also supports and provides resources to caregivers and family members navigating the patient’s illness.
The goal of palliative care is to manage symptoms, so patients feel the best they can throughout their illness, and families feel supported. Palliative care is patient centered and focused on the individual’s care goals and values.
Optimizing quality of life for patients and families is central to palliative care.
How does palliative care differ from hospice care?
Patients and families often confuse palliative care with hospice care. Our team works to dispel the misunderstanding by explaining our role and the ways we can help patients and families impacted by serious illness.
While both types of care focus on symptom management and comfort, palliative care is available to patients at any time and at any stage of illness. Hospice care is for patients at the end stages of an illness, with a life expectancy of six months or less.
Throughout their illness, palliative care patients receive treatment for their disease with the goal of improving their quality of life every day.
Hospice care comes in when curative treatments are no longer working, and the goal is to provide comfort and symptom relief for as long as the patient has.
Who can receive palliative care?
Anyone at any age, who has been diagnosed with a serious or chronic illness can receive palliative care, regardless of his or her prognosis.
While we meet some patients at the end of their disease, we also follow and care for other patients with chronic illness for many years.
These are patients living with heart, liver or kidney disease, cancer, dementia, Parkinson’s disease, Amyotrophic lateral sclerosis (ALS), chronic obstructive pulmonary disease (COPD) and other chronic conditions.
We are a hospital-based service but palliative care is also provided in outpatient clinics, skilled nursing and assisted living facilities and by some home care agencies. Patients interested in palliative care should speak with their provider.
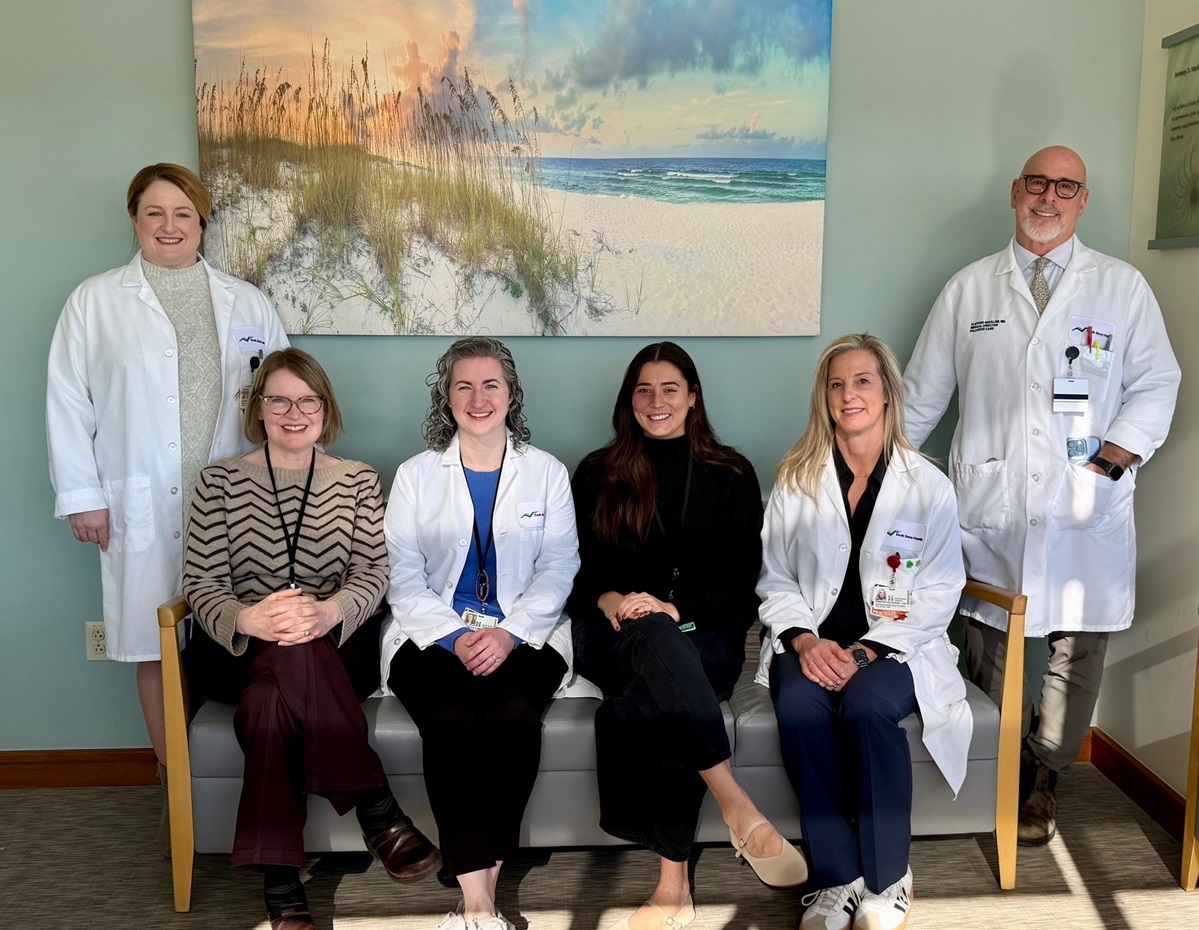
Who serves on South Shore Hospital’s Palliative Care Team and what roles do they play?
Our team of six includes medical director Clifford Breslow, MD, our chaplain, Rev. Cynthia Comiso, nurse practitioners Becky LaMay, DNP, AGACNP-BC and Dottie McCarron, MSN, FNP-C, ACHPN, physician assistant Alyson Hawkins, PA-C, BS, MPAS and clinical social worker Claudia Rizzo, LCSW.
We are a truly multidisciplinary team working to meet all of our patients’ needs – physical, emotional and spiritual.
Illnesses are complicated and there is more to every patient than what is in their chart.
Our patients usually see a combination of a provider, social worker and our chaplain depending on their needs. Our roles include providing symptom relief, social and spiritual support, and education and advocacy.
Educating patients and their families about their condition, how it may progress and how it could impact them in the future, is a big part of what we do as a team. We do a lot of expectation setting so we can help them through changes in their illness. By understanding their goals of care, we can better advocate for our patients.
As much medical knowledge as we have, that’s not the end of the line. There is so much more that our patients need that our team provides and doesn’t exist anywhere else.
What are some of the resources you provide for patients and families?
We offer a lot of support to children affected by a loved one’s illness. We provide young family members with stuffed animals, coloring books and books that help children understand complicated issues surrounding grief and death.
We also make fingerprint tokens for patients’ families. These individually designed glass tokens include the patient’s fingerprint and are a treasured keepsake for families. We provide as many fingerprint tokens a family requests.
Our team also connects patients and families with support groups, counseling services and other community resources they may need throughout their illness.
What are the rewards and challenges of being a palliative care provider?
The reward comes in knowing the positive impact we have had on patients and their families during a very difficult time. It is hard work, but knowing we have helped improve a patient’s quality of life and provided comfort, support, peace and dignity for their loved ones makes it rewarding and keeps us motivated to continue this work.
One of the challenges our team faces is when patients or families are in disagreement about a recommendation on how care should proceed. It’s difficult when we know that a choice or decision made will lead to suffering or pain, complications or hospitalization and negatively impact the patient’s quality of life.
We want patients to feel well as long as they can, but we can’t control everything. Ultimately, patients and their families have to make the decision that’s right for them and we have to honor that.
How do patients receive services from the palliative care team?
As an inpatient service, we get patient referrals from providers throughout the hospital, from the emergency department, intensive care unit, surgery and our hospitalists, to various specialties including nephrology, cardiology, and pulmonology. While our service is referral based, patients can request a consult by speaking with their provider.
During the consultation, our team assesses where the patient is with their illness, identifies symptoms they are dealing with and discusses goals of care and any specific needs they have including spiritual or psychosocial support.
Beyond medical problems, patients and their loved ones may have emotional and mental health needs. Family members, who are also caregivers, often struggle in a different way than the patient. Our multidisciplinary team works together to find out how we can help the entire family dynamic as they are going through an illness.
Alyson Hawkins, PA-C, BS, MPAS is a physician assistant and a member of South Shore Hospital’s Palliative Care Team.
Author

Alyson Hawkins, PA-C